SERVICES
At Harmony Superspeciality Hospital in Rajkot, our medical team and dedicated support staff provide high-quality gastroenterology services to include endoscopic procedures, management of gastrointestinal disorders, liver diseases and colorectal cancer screening.

Upper GI Endoscopy
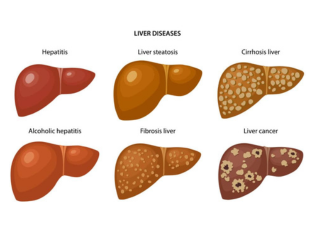
Alcohol Liver Disease

Gallstone

Rectal Bleeding

Pancreatitis
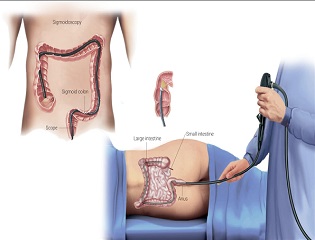
Colonoscopy

Abdominal Paracentesis

HBV Infections

Fatty Liver Disease
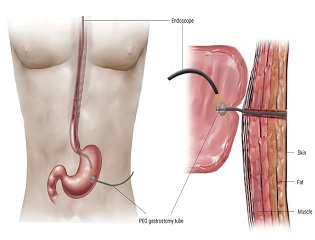
Percutaneous Endoscopic Gastrostomy
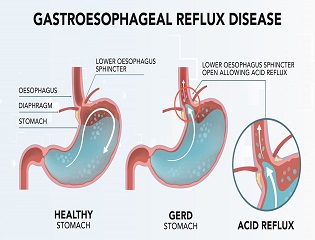
Gastroesophageal Reflux Disease

Belching, Bloating, Flatulence
Hepatitis A and-E

Ulcerative Colitis
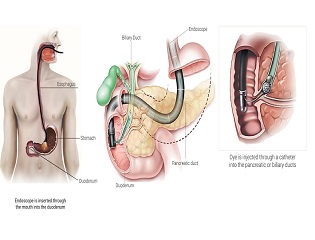
ERCP - Endoscopic Retrograde Cholangio - Pancreatography
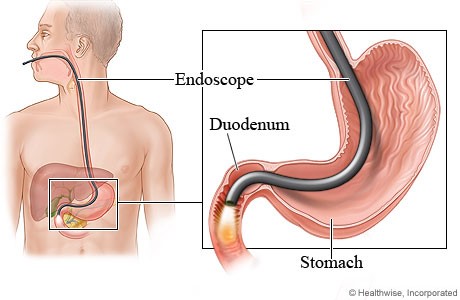
❈ What is upper endoscopy?
Upper endoscopy lets your doctor examine the lining of the upper part of your gastrointestinal tract, which includes the esophagus, stomach and duodenum (the first portion of the small intestine). Your doctor will use a thin, flexible tube called an endoscope, which has its own lens and light sou e, and will view the images on a video monitor.
❈ Why is upper endoscopy done?
Upper endoscopy helps your doctor evaluate symptoms of upper abdominal pain, nausea, vomiting or difficulty swallowing. It’s the best test for finding the cause of bleeding from the upper gastrointestinal tract. It is also more accurate than X-ray films for detecting inflammation, ultumoursnd tumors of the esophagus, stomach and duodenum. Your doctor might use upper endoscopy to obtain a biopsy (small tissue samples). A biopsy helps your doctor distinguish between benign (noncancerous) and malignant (cancerous) tissues. Remember, biopsies are taken for many reasons, and your doctor may take a biopsy even if he or she does not suspect cancer. For example, your doctor might use a biopsy to test for Helicobacter pylori, the bacterium that causes ulcers. Your doctor might also use upper endoscopy to perform a cytology test, where he or she will introduce a small brush to collect cells for analysis. Upper endoscopy is also used to treat conditions of the upper gastrointestinal tract. Your doctor can pass instruments through the endoscope to directly treat many abnormalities – this will cause you little or no discomfort. For example, your doctor might stretch (dilate) a narrowed area, remove polyps (usually benign growths) or treat bleeding.
❈ What preparations are required?
An empty stomach allows for the best and safest examination, so you should have nothing to eat or drink, including water, for approximately six hours before the examination. Your doctor will tell you when you should start fasting as the timing can vary. Tell your doctor in advance about any medications you take; you might need to adjust your usual dose for the examination. Discuss any allergies to medications as well as medical conditions, such as heart or lung disease.
Can I take my current medications? Most medications can be continued as usual, but some medications can interfere with the preparation or the examination. Inform your doctor about medications you’re taking, particularly aspirin products or antiplatelet agents, arthritis medications, anticoagulants (blood thinners such as warfarin or heparin), clopidogrel, insulin or iron products. Also, be sure to mention any allergies you have to medications.
What happens during upper endoscopy? Your doctor might start by spraying your throat with a local anesthetic or by giving you a sedative to help you relax.
You’ll then lie on your side, and your doctor will pass the endoscope through your mouth and into the esophagus, stomach and duodenum. The endoscope doesn’t interfere with your breathing. Most patients consider the test only slightly uncomfortable, and many patients fall asleep during the procedure.
❈ What happens after upper endoscopy?
You will be monitored until most of the effects of the medication have worn off. Your throat might be a little sore, and you might feel bloated because of the air introduced into your stomach during the test. You will be able to eat after you leave unless your doctor instructs you otherwise. Your physician will explain the results of the examination to you, although you’ll probably have to wait for the results of any biopsies performed. If you have been given sedatives during the procedure, someone must drive you home and stay with you. Even if you feel alert after the procedure, your judgment and reflexes could be impaired for the rest of the day.
❈ What are the possible complications of upper endoscopy?
Although complications can occur, they are rare when doctors who are specially trained and experienced in this procedure perform the test. Bleeding can occur at a biopsy site or where a polyp was removed, but it’s usually minimal and rarely requires follow-up. Perforation (a hole or tear in the gastrointestinal tract lining) may require surgery but this is a very uncommon complication. Some patients might have a reaction to the sedatives or complications from heart or lung disease. Although complications after upper endoscopy are very uncommon, it’s important to recognize early signs of possible complications. Contact your doctor immediately if you have a fever after the test or if you notice trouble swallowing or increasing throat, chest or abdominal pain, or bleeding, including black stools. Note that bleeding can occur several days after the procedure. If you have any concerns about a possible complication, it is always best to contact your doctor right away.
❈ What is a colonoscopy?
Colonoscopy lets your doctor examine the lining of your large intestine (colon) for abnormalities by inserting a thin flexible tube, as thick as your finger, into your anus and slowly advancing it into the rectum and colon. This instrument, called a colonoscope, has its own lens and light source and it allows your doctor to view images on a video monitor.
❈ Why is colonoscopy recommended?
The procedure is indicated in the following
- Unexplained changes in bowel habits.
- Bleeding from the back passage.
- Weight loss.
- Chronic constipation or chronic diarrhoea.
- History of polyps.
- Screening for cancer.
❈ What preparations are required?
Your doctor will tell you what dietary restrictions to follow and what cleansing routine to use. In general, the preparation consists of limiting your diet to clear liquids the day before and consuming either a large volume of a special cleansing solution or special oral laxatives. The colon must be completely clean for the procedure to be accurate and comprehensive, so be sure to follow your doctor’s instructions carefully.
❈ Can I take my current medications?
Most medications can be continued as usual, but some medications can interfere with the preparation or the examaination. Inform your doctor about medications you’re taking, particularly aspirin products, arthritis medications, anticoagulants (blood thinners such as warfarin or heparin), clopidogrel, insulin or iron products. Also, be sure to mention allergies you have to medications.
❈ What happens during colonoscopy?
Colonoscopy is well-tolerated and rarely causes much pain. You might feel pressure, bloating or cramping during the procedure. Typically, your doctor will give you a sedative or painkiller to help you relax and better tolerate any discomfort. You will lie on your side or back while your doctor slowly advances a colonoscope along your large intestine to examine the lining. Your doctor will examine the lining again as he or she slowly withdraws the colonoscope. The procedure itself usually takes less than 30 minutes, although you should plan on two to three hours for waiting, preparation and recovery. In some cases, the doctor cannot pass the colonoscope through the entire colon to where it meets the small intestine. Your doctor will advise you whether any additional testing is necessary.
❈ What if the colonoscopy shows something abnormal?
If your doctor thinks an area needs further evaluation, he or she might pass an instrument through the colonoscope to obtain a biopsy (a small sample of the colon lining) to be analyzed. Biopsies are used to identify many conditions, and your doctor will often take a biopsy even if he or she doesn’t suspect cancer. If colonoscopy is being performed to identify sites of bleeding, your doctor might control the bleeding through the colonoscope by injecting medications or by cauterization (sealing off bleeding vessels with heat treatment) or by use of small clips. Your doctor might also find polyps during colonoscopy, and he or she will most likely remove them during the examination. These procedures don’t usually cause any pain.
❈ What are polyps and why are they removed?
Polyps are abnormal growths in the colon lining that are usually benign (noncancerous). They vary in size from a tiny dot to several inches. Your doctor can’t always tell a benign polyp from a malignant (cancerous) polyp by its outer appearance, so he or she will usually remove polyps for analysis. Because cancer begins in polyps, removing them is an important means of preventing colorectal cancer.
❈ How are polyps removed?
Your doctor may destroy tiny polyps by fulguration (burning) or by removing them with wire loops called snares or with biopsy instruments. Your doctor will use a technique called “snare polypectomy” to remove larger polyps. Your doctor will pass a wire loop through the colonoscope and remove the polyp from the intestinal wall using an electrical current. You should feel no pain during the polypectomy.
❈ What happens after a colonoscopy?
You will be monitored until most of the effects of the sedatives have worn off. You might have some cramping or bloating because of the air introduced into the colon during the examination. This should disappear quickly when you pass gas. Your physician will explain the results of the examination to you, although you’ll probably have to wait for the results of any biopsies performed. If you have been given sedatives during the procedure, someone must drive you home and stay with you. Even if you feel alert after the procedure, your judgment and reflexes could be impaired for the rest of the day. You should be able to eat after the examination, but your doctor might restrict your diet and activities, especially after polypectomy. Your doctor will advise you on this.
❈ What are the possible complications of colonoscopy?
Colonoscopy and polypectomy are generally safe when performed by doctors who have been specially trained and are experienced in these procedures. One possible complication is a perforation, or tear, through the bowel wall. Bleeding might occur at the site of biopsy or polypectomy, but it’s usually minor. Bleeding can stop on its own or be controlled through the colonoscope; it rarely requires follow-up treatment. Some patients might have a reaction to the sedatives or complications from heart or lung disease. Although complications after colonoscopy are uncommon, it’s important to recognize early signs of possible complications. Contact your doctor if you notice severe abdominal pain, fever and chills, or rectal bleeding. Note that bleeding can occur several days after the procedure.
❈ What is Gastroesophageal Reflux Disease (GERD)?
Gastroesophageal reflux occurs when contents in the stomach flow back into the esophagus. This happens when the valve between the stomach and the esophagus, known as the lower esophageal sphincter, does not close properly.
❈ What are the symptoms of Gastroesophageal Reflux Disease?
Common symptoms of gastroesophageal reflux disease are heartburn and/ or acid regurgitation. Heartburn is a burning sensation felt behind the breast bone that occurs when stomach contents irritate the normal lining of the esophagus. Acid regurgitation is the sensation of stomach fluid coming up through the chest which may reach the mouth. Less common symptoms that may also be associated with gastroesophageal reflux include unexplained chest pain, wheezing, sore throat and cough, among others.
❈ What causes Gastroesophageal Reflux Disease?

Gastroesophageal reflux disease (GERD) occurs when there is an imbalance between the normal defense mechanisms of the esophagus and offensive factors such as acid and other digestive juices and enzymes in the stomach. Often, the barrier between the stomach and the esophagus is impaired by weakening of the muscle (lower esophageal sphincter) or the presence of a hiatal hernia, where part of the stomach is displaced into the chest. Hiatal hernias, however, are common and not all people with a hiatal hernia have reflux. A major cause of reflux is obesity whereby increased pressure in the abdomen overcomes the barrier between the stomach and the esophagus. Obesity, pregnancy, smoking, excess alcohol use and consumption of a variety of foods such as coffee, citrus drinks, tomato-based products, chocolate, peppermint and fatty foods may also contribute to reflux symptoms.
❈ How is Gastroesophageal Reflux Disease diagnosed?
When a patient experiences common symptoms of gastroesophageal reflux disease, namely heartburn and/or acid regurgitation, additional tests prior to starting treatment are typically unnecessary. If symptoms do not respond to treatment, or if other symptoms such as weight loss, trouble swallowing or internal bleeding are present, additional testing may be necessary. Upper endoscopy is a test in which a small tube with a light at the end is used to examine the esophagus, stomach and duodenum (the first portion of the small intestine). Before this test, you will receive medications to help you relax and lessen any discomfort you may feel. An upper endoscopy allows your doctor to see the lining of the esophagus and detect any evidence of damage due to GERD. A biopsy of tissue may be done using an instrument similar to tweezers. Obtaining a biopsy does not cause pain or discomfort. Another test, known as pH testing, measures acid in the esophagus and can be done by either attaching a small sensor into the esophagus at the time of endoscopy or by placing a thin, flexible probe into the esophagus that will stay there for 24 hours while acid content is being measured. This information is transmitted to a small recorder that you wear on your belt. X-ray testing has no role in the initial evaluation of individuals with symptoms of reflux disease.










Propping up the head of the bed at night may be helpful.
Should symptoms persist, over-the counter antacids may decrease discomfort. Antacids, however, only work for a short time and for this reason, they have a limited role in treating reflux disease. Histamine H2 receptor antagonists (such as cimetidine, ranitidine, nizatidine, and famotidine) decrease acid production in the stomach. These medications work well for treating mild reflux symptoms and are quite safe, with few side effects. They are available over the counter at a reduced dose, or at a higher dose when given by prescription by your doctor.
Proton pump inhibitors (such as omeprazole, lansoprazole, dexlansoprazole, pantoprazole, esomeprazole, and rabeprazole) are all highly effective in treating reflux symptoms. These medications act by blocking the final step of acid production in the stomach and are typically taken once or twice daily prior to meals. For reflux symptoms that occur frequently, proton pump inhibitors are the most effective medical treatment. These medications typically work well, are safe and have few side effects. There may possibly be an increased risk of certain side effects with high doses or with long-term use (over one year), however. You should discuss this with your doctor if you require long-term use or high doses.
Prokinetics, or medications that stimulate muscle activity in the stomach and esophagus, are sometimes provided for the treatment of reflux disease. The only available drug in the market is metoclopramide, which has little benefit in the treatment of reflux disease and has some side effects, some of which can be serious.
Surgery should be considered in patients with well-documented reflux disease who cannot tolerate medications or continue to have regurgitation as a primary symptom. If symptoms persist despite medical treatment, a comprehensive evaluation should be completed prior to considering surgery. The surgery for treating reflux disease is known as fundoplication. In this procedure, a hiatal hernia, if present, is eliminated and part of the stomach is wrapped around the lower end of the esophagus to strengthen the barrier between the esophagus and the stomach. The operation is typically done via a laparoscope, an instrument that avoids a full incision of the stomach. Due to the complexity of this surgery, it is important to seek a skilled surgeon who has experience in performing this procedure and can discuss the risks and benefits of the procedure.
❈ When should I see my doctor?
You should see your doctor immediately if you have symptoms such as unexplained weight loss, trouble swallowing or internal bleeding in addition to heartburn and/or acid regurgitation. Symptoms that persist after you have made simple lifestyle changes also warrant a visit to your doctor. In addition, if you use over-the-counter medications regularly to reduce symptoms such as heartburn or acid regurgitation, you should consult a physician to determine the best course of treatment for you.
❈ What is Alcohol Liver Disease?
Drinking alcohol consistently in moderate amounts over 10 to 20 years can cause alcohol liver disease. There are 3 types of liver conditions:
- Fatty liver
- Alcoholic hepatitis
- Cirrhosis
❈ Fatty liver
Accumulation of fat within liver cells in most people who drink regularly. Fatty liver usually causes no symptoms and is completely reversible if one stops drinking alcohol. However in some who continue to drink this can progress into hepatitis.
❈ Alcoholic hepatitis
It simple means inflammation of the liver. Ÿ Mild: Usually no symptoms, detected by blood tests showing abnormal liver enzymes. If this is persistent it can gradually damage the liver resulting in cirrhosis. This form of hepatitis can recover if one stops drinking completely. Ÿ Severe hepatitis: This tends to cause symptoms such as nausea, vomiting pain in the upper abdomen, jaundice( yellowing of the skin caused by high bilirubin level). In some cases this can lead to liver failure associated with clotting problems, bleeding, confusion , coma and can be fatal. Patients usually require admission and monitoring in hospital with complete abstinence from alcohol, proper nutrition along with supportive medical treatment. Some cases may need steroids or other antiinflammatory medication like pentoxyphylline. Unfortunately severe hepatitis has a poor outcome with only 50% chance of surviving beyond 3 months.
❈ Alcoholic Cirrhosis
Cirrhosis means scarring of liver, whereby normal liver tissue is replaced by scarred tissue(fibrosis). The liver becomes shrunken. This happens gradually if the liver tissue is inflamed for a long period of time. The liver is usually able to repair itself with complete abstinence from alcohol, however it never recovers completely. By stopping drinking you can prevent further damage to your liver and reduce risk of decomposition . This term is often used by liver specialist to suggest onset of complications from poor liver function. The following complications can be potentially fatal.
- Jaundice( yellow discolouration of eyes),
- Ascites(swollen belly due to water retention),
- Hepatic encephalopathy (confusion),
- vomiting of blood from varices (swollen internal veins)
- Liver cancer
- Hepatorenal syndrome: (poor kidney function due to liver disease)
- Malnutrition(poor intake of vitamins, minerals, protein from loss of appetite)
Most patients will require liver transplantation if there is no improvement in liver function after a period of abstinence from alcohol.
❈ How to prevent alcoholic liver disease?
- If you follow the recommended safe limits of alcohol consumption, you are unlikely to develop liver disease due to alcohol.
- Men: Should not drink more than 21 units of alcohol / week( and no more than 4 units in any one day)
- Women: should not exceed 14 units of alcohol/week (and no more than 3 units in any one day) Ÿ Pregnant women or women trying to conceive should avoid alcohol completely.
- Avoid binge drinking as this is harmful, although the weekly total may not appear to be high. (e.g taking one bottle of wine in a day or 4-5 pints of beer in a day)
❈ What is Abdominal Paracentesis?
It is also called ascitic tap. It is a procedure where a small needle is inserted through the abdominal wall to remove fluid from within the abdomen. Collection or accumulation of fluid in the spaces between the tissues and organs in the cavity of the abdomen is called ascites.
❈ Why do I need it?
This can be needed in 2 situations:
- Diagnostic tap: Where a small amount of fluid is removed and sent to the laboratory for analysis to evaluate the cause of ascites
- Therapeutic: To relieve the pressure from within your abdomen due to excess built of fluid resulting in tense ascites.
❈ What causes the fluid to accumulate in the abdominal cavity?
There are many causes for ascites. Commonest cause is due to underlying liver disease. Other causes:
- Cancer: cancer cells can spread to the lining of abdominal cavity and cause irritation resulting in build up of fluid
- Infection: Tuberculosis
- Heart failure
- Kidney problems: eg nephrotic syndrome
- Problems in lymphatic system etc.
❈ What are the symptoms?
- Swelling of the abdomen, with associated pain or discomfort.
- Discomfort during sitting or moving
- Breathlessness in case of tense ascites
- Tiredness.
- Nausea and vomiting
- Reduced appetite
❈ How is the procedure done?
- Your abdomen will be examined to determine the site for the paracentesis needle to be inserted. You may need an ultrasound scan to locate the area where the fluid has collected and this site is marked. Gel is placed on your abdomen and a small hand-held scanner moved across your skin. The ultrasound examination is painless.
- A blood test may be taken to check that your blood clots normally before the procedure is performed.
- This procedure can be done as a day case requiring you to stay in hospital for 6 hrs. However you may need to be admitted for overnight monitoring depending on your condition
- Before the procedure begins you will be asked to empty your bladder. • You will need to lie on your back . The doctor will give you a local anaesthetic (an injection to numb the skin). During the procedure, a needle will be inserted into your abdomen. The fluid (ascites) will drain through this needle into a drainage bag . The tube is usually removed once most of the fluid has been drained and a dressing is applied over the drainage site. You may experience slight discomfort during the procedure, but it should not be painful. Painkillers can be given if you experience any discomfort, inform the nursing staff if this occurs. Sometimes after the drainage has taken place, build up of fluid can occur again over a period of time. If this happens then paracentesis can be repeated.
❈ What are the benefits of paracentesis?
Having the fluid drained from your abdomen will relieve discomfort. The results of the test will help determine why the fluid is present.
❈ What are the risks associated with paracentesis?
- If a large quantity of fluid is removed, there is a slight risk of lowered blood pressure. Your blood pressure, pulse and temperature will be monitored regularly during your stay in hospital.
- The draining fluid can become blocked. If this happens you may be asked to move around, as this can sometimes clear the blockage. If this does not work then the needle might have to be removed and another one put in.
- There is a very small risk that your bowel might be punctured during the procedure. This is unlikely but may cause bleeding or infection and could require an operation.
❈ Are there any alternatives to paracentesis?
Some patients may benefit from a medication known as a diuretic, which will make you urinate more frequently than normal. This treatment is only suitable for certain patients and in these circumstances it may slow the build up of fluid in the abdomen.
❈ Overview
Intestinal gas is a topic that people often find difficult to discuss, but we all have gas in our intestinal tract. Gas can contribute to a sense of bloating (fullness), belching, abdominal cramps, and flatulence (gas). These symptoms are usually brief and resolve once gas is released by belching or flatulence. Some people can be more sensitive to even normal amounts of gas and develop the above symptoms.
❈ Symptoms
Belching is a normal process and results from swallowed air accumulating in the stomach. The air can either be belched back or can be passed out of the stomach into the small intestine and be subsequently passed as rectal gas (flatus).
Bloating refers to a sense of fullness in the upper abdomen. This can be influenced by gas and/or food accumulation in the stomach. Some patients experience the symptom with normal amounts of gastric gas.
Flatulence refers to the passage of rectal gas. The gas is generally a combination of swallowed air and gas produced by the action of colon bacteria on undigested carbohydrates.
Gas which accumulates in the right upper portion of the colon can lead to pain which could seem like gallbladder pain. Gas which accumulates in the left upper portion of the colon can radiate up to the chest and seem like cardiac pain.
❈ Risk Factors
As mentioned above, excessive air swallowing, and certain foods and carbonated beverages are significant contributors to belching and flatulence. Some patients with Irritable Bowel Syndrome (IBS) appear to be uniquely sensitive to normal or only slightly increased volumes of intestinal gas and may develop abdominal cramps as a result. Patients with altered anatomy due to surgery or those with certain rheumatologic diseases may be at an increased risk of bacterial overgrowth in the small intestine which can lead to belching, bloating or flatulence.
Some patients, particularly women who have had one or more pregnancies, experience abdominal distension when standing erect. This is often assumed to be gas accumulation. However, if the distension is not present when the patient is lying “flat”, then the likely explanation is weak abdominal muscles (which extend from the lower rib cage to the pelvis on both sides of the umbilicus) due to the stretching and loss of muscle tone which occurs during pregnancy.
❈ Diagnosis
There are individuals who have heartburn and stomach disorders that may swallow air for relief. The diagnosis of esophageal reflux or gastric inflammation should be excluded by x-rays or endoscopy (examining the esophagus and stomach with a flexible tube while the patient is sedated). Abdominal distension when erect but not when recumbent is an indication of weak abdominal muscles. If lactose intolerance is suspected, milk can be withdrawn from the diet and symptoms observed
However, lactose can be administered orally and the hydrogen gas which is generated in susceptible people can be measured in the breath. Postnasal discharge from sinus problems can cause air swallowing and should be considered. If bacterial overgrowth is suspected, your physician may administer a hydrogen breath test. Blood tests are not usually helpful for gaseous problems but testing for celiac disease may prove useful since failure to absorb wheat, barley, and rye can lead to excess flatulence.
Patients complaining of excessive gas passages may benefit from keeping a “flatus” diary for three days. The time of each gas passage and food for each meal can be noted. The gas passages can be compared to published “normal” flatus frequency.
❈ Treatment
Patients should eliminate carbonated beverages such as soda and beer. Foods such as cauliflower, broccoli, cabbage, beans, and bran should be avoided. Milk and other dairy foods should be avoided. Lactaid milk or non-dairy milk such as soy or almond milk can be used. Chewing gum and sucking on hard candies should be avoided. Sugar free gum and hard candies should be avoided as they may have mannitol or sorbitol as sweeteners which can cause flatulence. To ensure that only potentially symptom causing foods are eliminated without resulting in marked dietary restrictions, patients should eliminate food items one by one and keep a symptom diary.
Simethicone products have been promoted as treatment for gaseousness but their efficacy has not been convincing. Charcoal tablets have also been used to reduce flatulence without convincing benefit. Bismuth subsalicylate has been used to reduce the noxious odor of some sulfa-containing rectal gasses. Alpha-d-galactosidase, an over the counter product, has been used to help in the digestion of complex carbohydrates. Some patients may benefit from this strategy.
Individuals with IBS may benefit from symptomatic therapy for “gas pains” by using antispasmodic therapy such as dicyclomine or hyoscyamine under the tongue.
Some patients with bacterial overgrowth may see improvement from the occasional use of antibiotics to reduce the number of bacteria in the small bowel, thereby reducing gas production.
If weak abdominal muscles are suspected as a cause for abdominal distension, abdominal-tensing exercises may be helpful, although very difficult to achieve when patients are middle aged and older.
If symptoms fail to respond to the dietary strategies noted above, medical help should be sought to be confident that no other underlying abnormalities are present.
❈ IMPORTANT POINTS
- Belching and flatulence are normal body processes.
- Swallowed air is “gas” in the body and contributes significantly to symptoms.
- Unabsorbed dietary carbohydrates can cause gas production by colon bacteria.
- Carbonated beverages, sucking on hard candy, and chewing gum should be avoided.
- Abdominal distension when erect but not recumbent may be due to weak abdominal muscles.
- Increasing frequency or severity of symptoms should prompt medical attention.
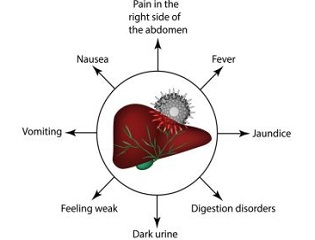
❈ Incidence and Risk Factors
Approximately 1 in 20 people may have gall stones.
About one in three women, and one in six men, form gallstones at some stage in their life.
The risk of forming gallstones increases with pregnancy, obesity, rapid weight loss.
However, they cause no symptoms in two out of three people (Asymptomatic gall stone disease)
❈ Understanding the gallbladder and bile

The gallbladder lies under the liver on the right side of the abdomen. It is a ‘reservoir’ which stores bile. The gallbladder empties the stored bile through the main bile duct into the duodenum.
Bile helps to digest food, particularly fatty foods
❈ What are gallstones?

There may be multiple small stones or a single large stone.
❈ What problems can gallstones cause?
Gallstones are often found when the abdomen is scanned for other reasons.
- Biliary colic: This is a severe pain in the upper abdomen.
- Inflammation of the gallbladder: This is called cholecystitis. This can lead to infection in the gallbladder. Symptoms usually develop quickly and include abdominal pain, high temperature (fever), and being generally unwell.
- Jaundice: It occurs if a gallstone gets stuck in the bile duct. Bile then cannot pass into the gut and hence causes jaundice
- Pancreatitis: This is an inflammation of the pancreas.
❈ How are gallstones diagnosed?

Ultrasound scan and blood tests are the most common investigations done. Other investigations like an MRI (MRCP) and Endoscopic Ultrasound (EUS) of the abdomen may sometimes be required
❈ What are the treatments for gallstones?
It is often best to leave gallstones alone if there are no symptoms. Symtomatic patients need surgery
Surgery
Keyhole surgery is now the most common way to remove a gallbladder. The medical term for this operation is laparoscopic cholecystectomy.
Rarely, if there are severe adhesions or unsafe to proceed with laparoscopic surgery, the operation may be converted to a traditional open cut method.
❈ WHAT ARE THE RISKS OR COMPLICATIONS OF THE SURGERY?
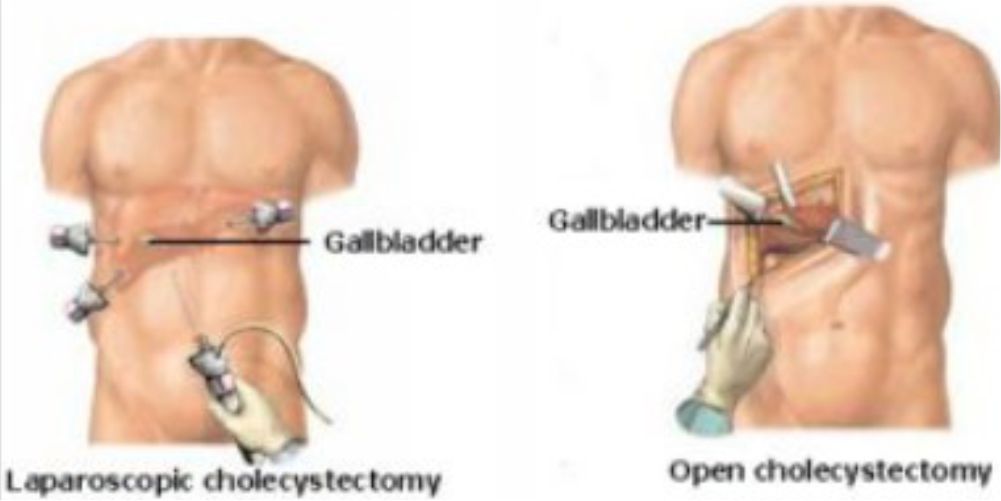
- Bleeding
- Damage to the blood vessels that go to the liver
- Infection in your belly
- Injury to the common bile duct
- Injury to the small intestine
- Pancreatitis (inflammation in the pancreas)
❈ AFTER THE PROCEDURE

If you do not have any signs of problems, you will be able to go home next day when you are able to drink liquids easily. If there are any problems like bleeding, or the patient is in a lot of pain, or a fever, you may need to stay in the hospital longer
❈ Are there any symptoms after a gallbladder is removed?
Some people who have had their gallbladder removed may develop mild abdominal pain or bloating from time to time.
❈ When will I be able to join work?
You need to take rest for 2-3 days at home (Not bed rest). Most people can join back work within 3-10 days.
Skin stiches would generally dissolve by itself. However, sometimes, sutures may need to be removed after 7-10 days.
❈ Hepatitis B is a virus passed from person to person by
- Blood to blood contact, i.e. needles or other medical equipment which is contaminated with infected blood, infected blood being spilt onto a wound & most imp Blood transfusion.
- Having sex with an infected person .
- Women who are hepatitis B positive can transmit the virus to their children .
- A human bite from an infected person.
- Household contacts: sharing toothbrushes or razors.
- Tattooing, ear piercing.
- Hemodialysis machine.
❈ What are the symptoms ?
Hepatitis B is a silent infection. Sometimes, in acute stage person may have the following symptoms:
- A short mild flu-like illness
- Feeling ill and tired
- Vomiting, diarrhoea and Weight loss
- Jaundice (yellow skin and eyes) and
- Pale stools and dark urine.
❈ Why have a test?
- If you are a carrier you can take steps to avoid passing it on to other people.
- If you are pregnant and a carrier of Hepatitis B, your baby can be protected by a vaccination soon after birth.
- If hepatitis B is left untreated, it can cause cirrhosis and liver cancer.
❈ How is Hepatitis B diagnosed?
Blood Test that includes :
- LFT ( Liver function test)
- Hepatitis B Surface antigen (HBsAg)
- Anti – core IgM (IgM anti – HBc)
- Hepatitis B Surface Antibody (HBsAb or anti – HBs )
- Hepatitis B Envelope Antigen (HBeAg)
- Hepatitis B Envelope Antibody (Anti-HBe or HBeAb):
- HBV DNA ( qualitative + quantitative )
- Ultrasound of the liver.
- Liver Biopsy : it is removal of small piece of tissue from the liver using a special needle. The tissue is examined under a microscope to look for inflammation or liver damage.
- Fibroscan which can be done instead of liver biopsy to assess the degree of damage to liver.
❈ Is there a vaccine?
❈ Treatment to prevent Hepatitis B infection after exposure?
❈ Treatment for Acute Hepatitis B infection?
If you have an acute infection , meaning it is short lived & can go away on its own & you may not need any treatment.
❈ What is Hepatitis A and E?
It is a virus that infects the liver causing inflammation of the liver.
❈ How is the infection acquired?
Hepatitis A or E is spread primarily through food or water contaminated by faeces from an infected person.
❈ Who is at risk for hepatitis A or E?
International travelers, particularly those traveling to developing countries.
❈ What are the symptoms of Hepatitis A or E?

- Tiredness
- Stomach upset
- Fever
- Loss of appetite
- Stomach pain, Diarrhoea
- Dark yellow urine
- Light coloured stool
- Yellowish eye & skin called jaundice
❈ How is Hepatitis A or E treated?
- Hepatitis A or E usually gets better in a few weeks without any specific antiviral treatment.
- Symptomatic treatment is given for itching, nausea, vomting due to jaundice. Patient is encouraged to drink bolied water and home cooked food. Avoid medications unless prescribed by a registered medical practitioner.
- Small percentage of patients, Hepatitis A or E (1% ) will develop acute liver failure.
- In pregnant patient with hepatitis E the risk of acute liver failure is 20%.
❈ How can Hepatitis A and E be prevented?
Sometimes history and clinical examination alone can raise suspicion of the diagnosis. However tests are done to confirm the same.

- The hepatitis A vaccine offers immunity to adults and children older than age 1. In India most people are exposed early and therefore vaccination is not routinely recommended.
- No vaccine for Hepatitis E, however, research is ongoing.
- Avoiding tap water when travelling internationally.
- Practising good hygiene and sanitation also help prevent hepatitis A or E.
Rectal Bleeding refers to the passage of a drops of bright red (fresh) blood from the rectum, which may appear on the stool, on the toilet paper or in the toilet bowl. Continuous passage of significantly greater amounts of blood from the rectum or stools that appear black, tarry or maroon in color can be caused by other diseases that will not be discussed here. Call your doctor immediately if these more serious conditions occur. Because there are several possible causes for minor rectal bleeding, a complete evaluation and early diagnosis by your doctor is very important. Rectal bleeding, whether it is minor or not, can be a symptom of colon cancer, a type of cancer that can be cured if detected early.
❈ What are hemorrhoids?
Hemorrhoids (also called piles) are swollen blood vessels in the anus and rectum that become engorged from increased pressure, similar to what occurs in varicose veins in the legs. Hemorrhoids can either be internal (inside the anus) or external (under the skin around the anus). Hemorrhoids are the most common cause of minor rectal bleeding, and are typically not associated with pain. Bleeding from hemorrhoids is usually associated with bowel movements, or it may also stain the toilet paper with blood. The exact cause of bleeding from hemorrhoids is not known, but it often seems to be related to constipation, diarrhea, sitting or standing for long periods, obesity, heavy lifting and pregnancy. Symptoms from hemorrhoids may run in some families. Hemorrhoids are also more common as we get older. Fortunately, this very common condition does not lead to cancer.
❈ How are hemorrhoids treated?
Medical treatment of hemorrhoids includes treatment of any underlying constipation, taking warm baths and applying an over-the-counter cream or suppository that may contain hydrocortisone. If medical treatment fails there are a number of ways to reduce the size or eliminate internal hemorrhoids. Each method varies in its success rate, risks and recovery time. Your doctor will discuss these options with you. Rubber band ligation is the most common outpatient procedure for hemorrhoids. It involves placing rubber bands around the base of an internal hemorrhoid to cut off its blood supply. This causes the hemorrhoid to shrink, and in a few days both the hemorrhoid and the rubber band fall off during a bowel movement. Possible complications include pain, bleeding and infection. After band ligation, your doctor may prescribe medications, including pain medication and stool softeners, before sending you home. Contact your doctor immediately if you notice severe pain, fever or significant rectal bleeding. Laser or infrared coagulation and sclerotherapy (injection of medicine directly into the hemorrhoids) are also office-based treatment procedures, although they are less common. Surgery to remove hemorrhoids may be required in severe cases or if symptoms persist despite rubber band ligation, coagulation or sclerotherapy.
❈ What are anal fissures?
Tears that occur in the lining of the anus are called anal fissures. This condition is most commonly caused by constipation and passing hard stools, although it may also result from diarrhea or inflammation in the anus. In addition to causing bleeding from the rectum, anal fissures may also cause a lot of pain during and immediately after bowel movements. Most fissures are treated successfully with simple remedies such as fiber supplements, stool softeners (if constipation is the cause) and warm baths. Your doctor may also prescribe a cream to soothe the inflamed area. Other options for fissures that do not heal with medication include treatment to relax the muscles around the anus (sphincters) or surgery.
❈ What is proctitis?
Proctitis refers to inflammation of the lining of the rectum. It can be caused by previous radiation therapy for various cancers, medications, infections or a limited form of inflammatory bowel disease (IBD). It may cause the sensation that you didn’t completely empty your bowels after a bowel movement, and may give you the frequent urge to have a bowel movement. Other symptoms include passing mucus through the rectum, rectal bleeding and pain in the area of the anus and rectum. Treatment for proctitis depends on the cause. Your doctor will discuss the appropriate course of action with you.
❈ What are colon polyps?
Polyps are benign growths within the lining of the large bowel. Although most do not cause symptoms, some polyps located in the lower colon and rectum may cause minor bleeding. It is important to remove these polyps because some of them may later turn into colon cancer if left untreated.
❈ What is colon cancer?
Colon cancer refers to cancer that starts in the large intestine. It can affect both men and women of all ethnic backgrounds and is the second most common cause of cancer deaths in the United States. Fortunately, it is generally a slow-growing cancer that can be cured if detected early. Most colon cancers develop from colon polyps over a period of several years. Therefore, removing colon polyps reduces the risk for colon cancer. Anal cancer is less common but curable when diagnosed early.
❈ What are rectal ulcers?
Solitary rectal ulcer syndrome is an uncommon condition that can affect both men and women, and is associated with long-standing constipation and prolonged straining during bowel movement. In this condition, an area in the rectum (typically in the form of a single ulcer) leads to passing blood and mucus from the rectum. Treatment involves fiber supplements to relieve constipation. For those with significant symptoms, surgery may be required.
❈ How is rectal bleeding evaluated?
Your doctor may examine the anus visually to look for anal fissures, cancer or external hemorrhoids, or the doctor may perform an internal examination with a gloved, lubricated finger to feel for abnormalities in the lower rectum and anal canal.If indicated, your doctor may also perform a procedure called colonoscopy. In this procedure, a flexible, lighted tube about the thickness of your finger is inserted into the anus to examine the entire colon. Sedative medications are typically given for colonoscopy to make you sleepy and decrease any discomfort. As an alternative, to evaluate your bleeding, your doctor may recommend a flexible sigmoidoscopy, which uses a shorter tube with a camera to examine the lower colon and rectum. To examine only the lower rectum and anal canal, an anoscope may be used. This very short (3 to 4 inch) tube is especially useful when your doctor suspects hemorrhoids, anal cancer or anal fissures.
❈ Non-alcoholic Fatty Liver Disease and Non-Alcoholic Steatohepatitis
Non-alcoholic fatty liver disease (NAFLD) is a condition in which fat builds up in the liver. In some cases this accumulation of fat can cause inflammation of the liver and eventually lead to permanent scarring (cirrhosis), which can seriously impair the liver’s ability to function. Unlike alcoholic fatty liver disease (alcoholic steatohepatitis), NAFLD can occur in people who drink no alcohol or drink only in moderation. NAFLD is, however, closely associated with obesity and diabetes. The consequences of the condition can be grave and NAFLD represents a major global public health problem.
❈ How to diagnose NAFLD?
A healthy liver contains very little or no fat. NAFLD occurs in people who do not drink a significant amount of alcohol (20 grams per day for men and 10 grams per day for women) and who do not have a viral infection or other specific cause of liver disease. NAFLD is diagnosed when accumulation of fat in the organ exceeds 5% of hepatocytes (the cells that make up the majority of the liver). NAFLD is sometimes called a ‘silent disease’ as even in its late stages it may have no symptoms and may only be diagnosed after liver function tests have revealed an abnormality.
❈ Diagnosis:
- Blood test (AST and ALT usually elevated)
- Imaging: Usually presence of fat seen on ultrasound, CT scan or MRI
- Liver biopsy
- Liver fibroscan (non-invasive test) has replaced liver biopsy in majority of case
❈ What are the stages of NAFLD and treatment options?
From simple fatty liver to irreversible cirrhosis NAFLD can progress from steatosis, to non-alcoholic steatohepatitis (NASH), to fibrosis and then to cirrhosis. Effective treatment options in NAFLD include weight reduction, dietary changes and physical activity. In its early stages, NAFLD can be treated through diet and lifestyle changes, such as losing weight. Cirrhosis, the most severe stage of NAFLD, usually only occurs after years of liver inflammation and can lead to a range of complications, including liver failure and hepatocellular carcinoma (HCC). Between 10 and 30% of patients with NAFLD have NASH that can progress to cirrhosis.
❈ What are the risk factors for developing NAFLD?
NAFLD is usually seen in people who are overweight or obese. Those with insulin resistance, type 2 diabetes, high blood pressure or high blood lipids (cholesterol and triglycerides) are also more likely to develop NAFLD. Studies have reported NAFLD prevalence rates of between approximately 43 and 70% in adults with type 2 diabetes. Obesity and diabetes are on the rise around the world. Obesity triggers inflammatory pathways in the brain and adipose tissue, resulting in the disruption of insulin levels. Over time, fat accumulates in the liver (as well as muscles and blood vessels), which exacerbates systemic insulin resistance.
❈ The heavy toll of NAFLD
NAFLD increases the risk of overall mortality and of mortality related to cardiovascular disease and liver disease. Controlling the etiological factors helps to reverse the condition as long as there is no permanent scarring in the liver. Persistent inflammation can cause scarring and cirrhosis.
❈ What is Ulcerative Colitis?
Ulcerative colitis (UC) is a disease marked by inflammation of the lining of the colon and rectum, together known as the large intestine. This inflammation causes irritation in the lining of the large intestine which leads to the symptoms of UC. Though UC always affects the lowest part of the large intestine (the rectum), in some patients it can be present throughout the entire colon. UC belongs to a group of diseases called inflammatory bowel diseases which also includes Crohn’s disease (CD). Though it was once thought that UC and CD were two different diseases, as many as 10% of patients may have features of both diseases and this is called indeterminate colitis. It is important to note that inflammatory bowel disease (IBD) is different from irritable bowel syndrome (IBS).
❈ What are the symptoms of UC?
The symptoms of ulcerative colitis depend on the severity of inflammation and the amount of the colon that is affected by the disease. In patients with mild to moderate inflammation, symptoms can include rectal bleeding, diarrhea, mild abdominal cramping, stool urgency, and tenesmus (discomfort and the feeling that you have not completely emptied your rectum after a bowel movement). When more severe inflammation is present, patients often develop fever, dehydration, severe abdominal pain, weight loss, loss of appetite or growth retardation (in children and adolescents with UC). Individuals with moderate or severe inflammation may also have to wake up at night to have bowel movements and may lose control of bowel movements. Some of the symptoms of UC may be non-specific and could be caused by other diseases such as Crohn’s disease, irritable bowel syndrome, or infection. Your doctor can help determine the cause of your symptoms and should be consulted should you experience a significant change in your symptoms.
❈ How is UC diagnosed?
Your doctor will usually suspect the diagnosis of ulcerative colitis based on your symptoms, but confirmation of the diagnosis requires testing. Blood work is often checked to look for markers of inflammation or anemia (low blood counts), though these tests can be normal in patients with mild disease. Tests of your stool to look for evidence of an intestinal infection are often obtained. Radiologic images including x-rays and CT scans are usually not recommended but may be performed. All patients with symptoms consistent with UC should have a colonoscopy or flexible sigmoidoscopy to confirm the diagnosis assuming that they are healthy enough to undergo the procedure. During this procedure, your gastroenterologist will be able to directly examine the lining of your colon and rectum to look for evidence of inflammation and take small biopsies to be examined under a microscope to look for the cause of the inflammation.
❈ What causes UC?
The way in which patients get ulcerative colitis is still poorly understood. There seems to be an interaction between the unique genetic makeup of an individual, environmental factors, and a patient’s specific immune system that triggers the disease. UC is not an infection that can be passed from person to person. UC is an immune-mediated disease in which there is loss of control of the normal bowel immune activity and the ongoing activity results in damage to the bowel wall. Men and women are equally affected by UC.
UC is more common in first degree relatives (siblings, parents, and children) of patients affected by UC and up to 20% of patients will have an affected family member. Despite the influence of genetics, the majority of patients with UC do not pass the disease to their children. There is no way to predict those at higher risk. Individuals having their appendix removed prior to the age of 20 appear to be at lower risk of developing UC. No specific infectious agent has been linked to UC and diet, breast feeding, and various medications have also been examined but none have been found to cause UC.
It has been observed that smokers have lower rates of UC than non-smokers. Furthermore, those who smoke and have UC tend to have a milder course of UC than those who do not smoke (note that this is the exact opposite effect that smoking has on Crohn’s disease). Despite the protective role smoking appears to have on the development and natural history of UC, it is not recommended that patients start smoking to prevent UC due to the fact that there are so many other illnesses and cancers in which smoking is a definite risk factor.
❈ What are the possible complications of UC?
The complications of ulcerative colitis can be divided into those affecting the colon and those occurring outside of the colon. Within the colon, UC can rarely lead to toxic megacolon or colon cancer.
Toxic megacolon describes a severe disease flare with a high risk of infection and colonic perforation (holes in the colon). Patients may occasionally present with toxic megacolon as their initial presentation of UC and this complication requires hospitalization and may lead to surgery to remove the colon (colectomy). UC is known to increase the risk of colon cancer. Those patients who have had UC for a long time and those with a longer length of the colon affected are at higher risk of developing colon cancer. In general, patients begin to have an increased risk of colorectal cancer 10 years after the onset of disease symptoms and should have colonoscopy every one or two years starting at this time. Colon cancer is a rare complication and it is thought that it may be preventable based on control of inflammation of the colon and careful colonoscopy examinations that look for any pre-cancerous changes called dysplasia. Overall, the risk of colon cancer increases 0.5% yearly after 10 years of disease though patients with inflammation throughout their colon may be at higher risk. Those patients with primary sclerosing cholangitis (PSC) are at greatest risk for colon cancer and need to start screening upon diagnosis.
Patients with UC are also at risk for extra-intestinal manifestations of UC (complications outside of the colon). These complications most frequently involve the liver, skin, eyes, mouth, and joints. Within the liver, patients with UC may develop primary sclerosing cholangitis. This occurs in about 3% of patients with UC. PSC can progress even if UC is not active and it is often detected by elevations in liver blood tests and confirmed by the use of MRI scans such as Magnetic Resonance Cholangiopancreatography (MRCP) or endoscopic procedures such as Endoscopic Retrograde Cholangiopancreatography (ERCP).
Patients with UC can develop sores in the mouth or rashes on the skin that generally only appear when UC colon symptoms are active. The most common rashes that are seen in UC are erythema nodosum (EN) and pyoderma gangrenosum (PG). EN usually presents as a red, raised, painful area most commonly on the legs and is most often seen during flares of UC. PG also presents as raised lesions on the skin (most frequently on the legs) that often develops after trauma to the skin and can lead to the formation of ulcers. Unlike in EN, the appearance of skin lesions in PG may or may not mirror the activity of bowel symptoms. The eyes can become red and painful (uveitis) and vision problems should be reported to your doctor.
Arthritis is commonly associated with UC and can affect either small (such as the fingers/toes) or large joints (often the knee), though involvement of the smaller joints may have a course that is not related to activity in the colon. The joints of the spine can be affected as well, though this is less common than it is in Crohn’s disease.
As in other chronic medical conditions, anxiety and depression are common in patients with UC. The unpredictability of UC and the need to take medications on a daily basis can lead to feelings of frustration or anger. Though occasional feelings of frustration can be normal, feelings of significant anxiety or depression should be brought to the attention of your physician.
❈ What is the clinical course of UC?
Ulcerative colitis can present in a variety of ways. UC is often a chronic, life-long condition. It most often is diagnosed in the 2nd and 3rd decades of life (ages 11-30), although it can be diagnosed at any age. The initial presentation can be mild and is sometimes confused with other conditions such as irritable bowel syndrome or it can be very severe and require hospitalization and surgery. For most patients, UC tends to follow a course marked by periods of disease activity followed by variable periods during which a patient symptom-free. Some patients may have continuous disease activity. Rarely, a patient will have only a single disease flare. In general, those people with a severe first attack of UC and those who have their entire colon affected by UC tend to have a more aggressive course with more frequent flares and shorter periods of remission. Despite the chronic nature of UC, most patients are able to function well and the life expectancy of a patient with UC is normal.
❈ How is UC treated?
Medical treatment of ulcerative colitis generally focuses on two separate goals: the induction of remission (making a sick person well) and the maintenance of remission (keeping a well person from getting sick again). Surgery is also a treatment option for UC and will be discussed separately. Medication choices can be grouped into four general categories: aminosalicylates, steroids, immunomodulators, and biologics.
Aminosalicylates are a group of anti-inflammatory medications (sulfasalazine, mesalamine, olsalazine, and balsalazide) used for both the induction and maintenance of remission in mild to moderate UC. These medications are available in both oral and rectal formulations and work on the lining of the colon to decrease inflammation. They are generally well tolerated. The most common side effects include nausea and rash. Rectal formulations of mesalamine (enemas and suppositories) are generally used for those patients with disease at the end of their colon.
Steroids (prednisone) are an effective medication for the induction of remission in moderate to severe UC and are available in oral, rectal, and intravenous (IV) forms. Steroids are absorbed into the bloodstream and have a number of severe side effects that make them unsuitable for chronic use to maintain remission. These side effects include cataracts, osteoporosis, mood effects, an increased susceptibility to infection, high blood pressure, weight gain, and an underactive adrenal gland.
Immunomodulators include medications such as 6-mercaptopurine and azathioprine. These are taken in pill form and absorbed into the bloodstream. They are effective for maintenance of remission in moderate to severe ulcerative colitis, but are slow to work and can take up to 2-3 months to reach their peak effect. Because of this, these medications are often combined with other medications (such as steroids) in patients who are very ill. These medications require frequent blood work as they can cause liver test abnormalities and low white blood cell counts, both of which are reversible when the medication is stopped. Adverse reactions can include nausea, rash, liver and bone marrow toxicity, pancreatitis, and rarely lymphoma.
Biologic agents are medications given by injection that are used to treat moderate to severe UC. At the current time, infliximab (Remicade®) is the only biologic agent approved for use in UC, but other biologics used for Crohn’s disease under evaluation for the treatment of UC include adalimumab (Humira®), and certolizumab pegol (Cimzia®). Infliximab is effective in both the induction and maintenance of remission in UC. The side effects of this medicine may include an allergic reaction to the medication called an “infusion reaction” or “hypersensitivity reaction”. There are also rare risks of serious infections with these medications. Lymphoma is a rare risk of these therapies as well. Combination therapy with azathioprine/6-mercaptopurine and biologics increases the risk of a particularly rare type of lymphoma called hepatosplenic T-cell lymphoma. As with all medications, you should discuss the risks and benefits with your doctor.
Other medications used less frequently for UC include cyclosporine and tacrolimus. These agents are sometimes used in those rare cases of severe UC that are not responsive to steroids. Side effects of these agents include infections and kidney problems. These agents are offered at a limited number of hospitals and are usually used for a short period of time as a bridge to other maintenance therapies such as azathioprine or 6-mercaptopurine.
No matter which medical therapy you and your doctor decide upon, adherence with the prescribed course is essential. No medical therapy can work if it is not taken and failure to take your medications can lead to unnecessary escalation of therapy if it is not brought to the attention of your doctor. Because many of the complications associated with UC are related to ongoing disease activity, good medication adherence may minimize these risks.
❈ What is the role of surgery?
Surgery in ulcerative colitis is performed for a number of reasons and is generally considered to be curative if the entire large intestine removed. Patients who do not respond to medications, are concerned about or have unacceptable side effects from medications, develop toxic megacolon, dysplasia (precancerous lesions) or cancer, or children who are not growing because of UC are often considered for surgery. Several different surgeries are performed for UC and the choice of surgery is dependent on patient preference and the experience of the surgeon. The most common surgery is total proctocolectomy with ileal pouch-anal anastomosis (total removal of the colon and rectum with creation of a pseudo-rectum from a portion of the small intestine). This operation usually requires two separate surgeries to complete although it may require three stages in severely ill patients. Following this surgery, patients can expect 5-10 stools daily as they no longer have a colon to store stool. Patients usually feel better because their sense of stool urgency improves, they no longer have bleeding, and their medications can often be stopped. However, these patients are at risk for post-operative inflammation of the pouch known as pouchitis which is usually treated with antibiotics. Women who have this surgery may have decreased ability to get pregnant naturally.
Another common surgical procedure involves a proctocolectomy with ileostomy (removal of the entire colon and rectum and connection of the small intestine to the abdominal wall so that stool empties into a bag). This procedure is often undertaken in elderly patients, obese patients or those with anal dysfunction. Should you need a surgical procedure for UC, your surgeon can help you decide which type of surgery best fits your needs.
❈ Do complementary and alternative therapies work in UC?
Outside of the standard medical therapies discussed for ulcerative colitis, many alternative therapies have been studied. No studies have suggested that diet can either cause or treat UC and there is no specific diet that patients with UC should follow though it is advisable to eat a balanced diet. Likewise, there is no convincing evidence that UC results from food allergies. Though vitamin and mineral deficiencies are more common in Crohn’s disease, specific deficiencies can occur in UC patients. For this reason, a multivitamin and a calcium supplement are not unreasonable. Malnutrition can become a concern in severe UC.
Probiotics are species of bacteria that are thought to have beneficial properties for the bowel. There are a number of scientific studies which have been performed to assess the role of probiotics in UC, and most of these have not shown benefit. There is some evidence, however, that a specific probiotic (VSL #3) may be helpful as an additive to other therapies for maintenance of remission.
Various other herbal remedies and alternative therapies have been studied for use in patients with IBD such as curcumin (a derivative of the herb tumeric) and parasitic worms (helminths). Though limited studies have shown promise for a number of alternative therapies, these have not yet been shown to be safe and effective and are not currently recommended.
❈ What type of follow-up is required?
As mentioned earlier, ulcerative colitis is a chronic disease and establishing a long term relationship with a gastroenterologist experienced in the treatment of UC is advisable. Many medications used in UC require regular blood work to ensure that they are not causing any serious side effects. Patients with UC have a higher risk of osteoporosis associated with both underlying disease activity and long term or frequent steroid use. Because of this risk, your doctor may recommend measurement of Vitamin D blood levels and a bone mineral density screening with a DEXA scan. Colorectal cancer screening is also important because of the higher risk of cancer in patients with UC as discussed earlier.
❈ What is the pancreas?
The pancreas is in the upper abdomen and lies behind the stomach and guts (intestines). It makes a fluid that contains chemicals (enzymes) that are needed to digest food. The enzymes are made in the pancreatic cells and are passed into tiny tubes (ducts). These ducts join together like branches of a tree to form the main pancreatic duct. This drains the enzyme-rich fluid into the part of the gut just after the stomach (called the duodenum). The enzymes are in an inactive form in the pancreas (otherwise they would digest the pancreas). They are ‘activated’ in the duodenum to digest food.
Groups of special cells called ‘Islets of Langerhans’ are scattered throughout the pancreas. These cells make the hormones insulin and glucagon. The hormones are passed (secreted) directly into the bloodstream to control the blood sugar level.
The bile duct carries bile from the liver and gallbladder. This joins the pancreatic duct just before it opens into the duodenum. Bile also passes into the duodenum and helps to digest food.
❈ What is pancreatitis?
Pancreatitis means inflammation of the pancreas. There are two types:
Acute pancreatitis – when the inflammation develops quickly, over a few days or so. It often goes away completely and leaves no permanent damage. Sometimes it is serious.
Chronic pancreatitis – when the inflammation is persistent. The inflammation tends to be less intense than acute pancreatitis but as it is ongoing it can cause scarring and damage
❈ What are the causes of acute pancreatitis?
Gallstones or alcohol cause more than 8 in 10 cases.
- Gallstones – A gallstone can pass through and get stuck at the lower end of the bile duct, thus irritating the pancreas and causing an acute attack of pancreatitis.
- Alcohol – Heavy intake over a longer duration or binge drinking can cause a severe attack.
Uncommon Causes
- Viral infections like mumps
- High Triglyceride levels
- High calcium levels
- Autoimmune – this is where your own immune system attacks the pancreas
- Unknown – no cause is found in about 2-5 % of cases. However, a number of these cases are probably due to tiny gallstones or ‘gallstone sludge’ that passes through the bile duct.
❈ What happens in acute pancreatitis?
- In the majority of the cases, the inflammation is mild and settles within a week.
- Around 20% the attack is severe and causes damage to other organs. This can lead to shock, respiratory failure, kidney failure and other complications.
❈ What are the symptoms of acute pancreatitis?
- Abdominal pain
- Vomiting
- Backache
- Fever
- Feeling unwell
❈ How is acute pancreatitis investigated?
A combination of tests will help to detect the cause and assess the severity of the attack.
- Blood tests ( including amylase and lipase levels)
- CT scan of the abdomen or MRI (MRCP)
- Depending on the reports- a score can be calculated to quantify the severity of pancreatitis
❈ What is the treatment for acute pancreatitis?
- Patient will need hospitalization to the hospital. Sometimes the patient will need ICU stay.
- Mainline of treatment includes painkillers, antibiotics and intravenous fluids
- Surgery is sometimes needed to remove infected or damaged tissue.
- Removal of the gallbladder is advised if a gallstone was the cause.
- If it is secondary to alcohol, the patient will need to completely abstain from alcohol
- High triglyceride levels may need medications
❈ What is the outlook (prognosis) for acute pancreatitis?
As mentioned, acute pancreatitis is classified as mild if no complications develop (about 4 in 5 cases). In this case the outlook is very good and full recovery is usual.
Severe acute pancreatitis (about 1 in 5 cases) means that one or more complications develop. Despite intensive care treatment, up to a quarter of people with severe acute pancreatitis die.
❈ Will it happen again?
An attack of acute pancreatitis may be a one-off event. However, if there is an underlying cause, then it may recur unless the cause is corrected. One of the following may be relevant to prevent a recurrence, depending on the cause:
- An operation to remove your gallbladder is usually advised if a gallstone was the cause.
- Alcohol-related concerns: You should not drink alcohol for at least several months after a bout of acute pancreatitis, even if alcohol was not the cause of your pancreatitis. If alcohol is the cause of pancreatitis, you should stop drinking alcohol altogether. Sometimes a pancreatitis is the first indication of an alcohol dependency problem. Further help, advice and counseling may be offered to you if this is the case. It can be very difficult to stop drinking without some extra support.
- A high blood fat level (hyperlipidaemia) is sometimes the cause. This may need treating with medication.
- A side-effect from some medication is a rare cause of acute pancreatitis. A change in your medication may be needed if this is your cause of pancreatitis.
CHRONIC PANCREATITIS
❈ What are the causes of chronic pancreatitis?
- Alcohol – is the commonest cause (about 7 in 10 cases). In most cases the person has been drinking heavily for 10 years.
- Autoimmune – this is where your own immune system attacks the pancreas.
- Genetic – there are some rare genetic conditions like cystic fibrosis which can lead to chronic pancreatitis.
❈ What are the symptoms of chronic pancreatitis?
- Abdominal pain – spreading through to the back. Eating often makes the pain worse. Patient gets several recurrent episodes of pain and may need repeated admissions
- Weight loss- fear of eating leads to weight loss.
- Poor digestion (malabsorption) – Undigested fat from the diet is passed with stools. This causes pale, smelly, loose stools that are difficult to flush away (steatorrhoea).
- Diabetes – occurs in about 1 in 3 cases. This occurs when the pancreas cannot make sufficient insulin.
❈ What happens in chronic pancreatitis?
- A persistent inflammation develops in the pancreas.
- Inflammation causes damage to parts of the pancreas.
- Leads to inadequate production of digestive enzymes and insulin causing malabsorption of food and diabetes.
- Stone formation within the pancreatic duct.
❈ How is chronic pancreatitis diagnosed?
- There is no single test to detect chronic pancreatitis.
- Simple blood tests like blood count, Liver and Kidney profile, Blood sugar testing
- Stool test for fat content
- CT scan and/or MRI of the abdomen
❈ What are the complications that can develop?
- Pseudo-cyst – This is when pancreatic fluid collects into a cyst due to a blocked tube.
- Pancreatic duct stones- Due to excessive calcium deposition.
- Blockage of the bile duct -this can cause jaundice.
- Cancer of the pancreas – The risk increases in smokers and with increasing age.
❈ What is the treatment for chronic pancreatitis?
- Stop alcohol and smoking
- Painkillers – Apart from painkillers, other techniques to block the pain may be considered, such as celiac axis nerve blocks to the pancreas. (can be done through transcutaneous or with endoscopic sonography)
- Enzyme replacement medication.
- Dietary restrictions.
- Diabetes treatment- may need insulin injections.
- Surgery- Especially if there are pancreatic duct stones, pseudocyst or suspicion of cancer.
❈ What is a PEG?
A percutaneous endoscopic gastrostomy (PEG) is a procedure for placing a feeding tube directly into the stomach through a small incision in the abdominal wall with the assistance of an instrument known as an endoscope. The procedure is performed as a means of providing nutrition to patients who cannot take food by mouth. Many stroke patients, for example, have poor control over their swallowing muscles and are unable to safely consume enough food, or they have muscle weakness that allows food to leak into the lungs when they swallow things by mouth. Many of these patients will benefit from a PEG tube in order to receive adequate nutrition and to prevent them from respiratory problems that develop when food or fluids accidentally gets into the lungs.
❈ What are the medical indications for a PEG?
A PEG should be considered for pediatric and adult patients who are unable to consume sufficient food by mouth to meet their daily needs. These patients should be able to digest and absorb their food once it arrives in the stomach. The most common medical conditions requiring a PEG feeding tube are neurologic conditions associated with poor swallowing, such as experienced by stroke patients, and patients with cancers of the oral cavity or esophagus that prevent them from swallowing.
Other diseases of the esophagus that decrease a patient’s ability to swallow are also common indications for placing a PEG feeding tube. Patients with Alzheimer’s disease often lose their ability to swallow near the end of their life expectancy. The benefit of PEG tube placement in this patient group remains controversial. When a patient is being considered for PEG tube placement, the patient’s life expectancy and quality of life after the tube is placed should be considered to determine if placement of a feeding tube is appropriate.
❈ What is the medical procedure for placing a PEG tube?
PEG tubes are placed with the aid of an endoscope, an instrument to see inside your stomach and intestines. The patient receives sedatives and pain medications to make them comfortable. After confirming proper location and preparing the abdominal wall, a small incision is made in the abdomen. The PEG feeding tube is placed though this incision into the stomach. The procedure takes 15 to 20 minutes.
❈ Is there discomfort after the procedure?
There will be some minimal discomfort after the procedure from either cramping from gas in the digestive system or pain at the incision site itself. This pain can be well controlled with pain medication if required.
❈ Will the tube fall out once it is placed?
The tube is prevented from coming out of the stomach by one of several methods. Some commercial PEG brands have a mushroom-shaped cap on the end of the feeding tube inside the stomach. This cap is 2-3 times the diameter of the feeding tube. This cap is also called the internal bolster or internal bumper. Other systems employ a balloon at the end of the tube which is inflated once the tube is inserted, serving the same purpose. These internal bolsters prevent the PEG feeding tube from falling out.
❈ What does the PEG tube look like on the outside after placement?
The PEG tube has a diameter size about the same as a writing pen. Approximately 6 to 12 inches of tubing will protrude from the incision area. There will be a disc or a tubular device placed around the feeding tube lying against the abdominal wall. This is known as the external bolster or external bumper. It is meant to keep the tube from migrating forward into the stomach. At the outside end of the feeding tube is a capped plug. It may be a one hole or two hole plug. The plug is meant to be closed to prevent stomach content from getting on the skin and clothes of the patient. It is opened to allow food, medications and water to be placed through the PEG feeding tube. Suctioning of air and stomach contents can also be performed.
❈ What are the complications of a PEG tube?
Complications from this procedure may occur. Minor complications include leakage of food or fluid around the tube onto the abdominal wall surface, pain at the incision site, mild bleeding at the incision site or infection at the incision site. You should consult with your doctor if this occurs. Major complications are rare but can occur and include major bleeding, peritonitis (an infection inside the abdominal cavity) and damage to the colon or other surrounding organs. Delayed complications include “buried bumper” syndrome in which the internal bolster buries itself into the stomach wall. This can be avoided by not tightening the bolster too tightly.
❈ Are there alternatives to PEG?
There are alternatives to PEG feeding tubes. Nasogastric (NG) feeding tubes are tubes passed through the nose into the stomach for feeding. It is secured to the face with tape. Long-term use of these tubes can cause irritation, infection or bleeding of the nose and throat. These tubes also have a tendency to be accidentally pulled out. Also, a surgeon can place a feeding tube into the stomach in the operating room or a radiologist can place a feeding tube into the stomach in the fluoroscopy (X-Ray) suite. Similar procedures can be done to place feeding tubes into the jejunum as well, depending on the clinical scenario.
❈ How do you take care of a PEG tube?
The area around the incision on the abdominal wall should be cleaned daily and the incision may be covered with clean gauze. Often, these gauze sponges have a slit in them so they can be placed around the PEG tube, over the incision. The tube itself has centimeter markings written on the side. The centimeter marking at or near the incision site should be noted. If this number changes, the tube should be readjusted back to the original centimeter marking. The external bolster should rest gently near the abdominal wall. This external bolster should not be placed too tightly against the abdominal wall or it may lead to infection or skin ulceration.
Should the tube accidentally come out, it must be replaced within twenty-four hours or the incision may begin to close and new PEG procedure may be required. If the tube falls out, a physician should be contacted as soon as possible. A urinary (Foley) catheter can be temporarily inserted into the track to keep it open until a standard PEG tube can be replaced. If the tube needs removal or replacement, it is usually wise to wait 6 or more weeks after insertion before removal.
❈ What exact nutritional formula is placed through the PEG tube?
After the PEG feeding tube is placed, a registered dietician, nurse or physician who specializes in nutrition should assess the patient to determine their nutritional needs; this means the amount of calories, protein, and fluids that will be necessary each day, as well as the most appropriate nutritional formula. Nutritional products designed for tube feeding are formulated to provide all the nutrients the patient will need including vitamins, and minerals.
❈ How is a PEG tube used for feeding?
The PEG tube is relatively narrow. Commercial tube feedings are available and are designed to reduce the risk of tube clogging. The PEG tube should be flushed with water before and after feedings, or after medications have been administered. The placement of table foods into the PEG tube is discouraged as it can lead to tube clogging. It is imperative that the caregiver or patient thoroughly washes their hands with soap and water before preparing formula or having contact with the PEG system.
The commercial tube feeding formula is administered at room temperature. The patient should be upright, no less than thirty degrees, to minimize the risk of regurgitation and potential aspiration (tube feeding getting into the lungs). The patient should be kept upright for thirty to sixty minutes after feeding. To prevent complications (abdominal cramping, nausea and vomiting, bloating, diarrhea, aspiration), tube feeding should be infused slowly.
The simplest method of infusing tube feeding through the PEG tube is called bolus feeding. Tube feed formula is placed within a large syringe and slowly administered to the patient through the plug cap on the end of the PEG feeding tube. In order to meet a patient’s nutritional needs, this may need to be repeated 4 to 6 times per day. Sometimes continuous feeding is preferable. With this method, a feeding pump is set up and connected to the PEG tube. The tube feed formula is placed in a large bag and attached to the pump. The tube feeding is continuously administered by the pump over 12-24 hours.
❈ Can I put medications through a PEG tube?
Most medications that come in tablet or pill form can be crushed and dissolved in water and passed through the feeding tube. In addition, there may be liquid formulations of medications that can be prescribed. However, some capsules are designed to dissolve within various portions of the gastrointestinal tract and therefore cannot be broken up. The tube should be flushed with water after introduction of medication to prevent clogging. Ask your doctor about specific medications.
❈ Is a PEG tube permanent?
Depending on the medical condition, a PEG feeding tube may be temporary or permanent. After a minor stroke, for example, a patient may recover swallowing and ultimately be able to get adequate calories and nutrients from eating by mouth. However, those with more permanent neurologic damage may require a feeding tube long-term. In either case, the feeding tube can be easily removed if necessary.
❈ Do PEG feeding tubes last forever?
The lifespan of the PEG feeding tube is about 1 year although the tube may wear out sooner. When the tubing begins to wear, you will notice pits, bumps and leaks on the side of the tube. In addition, the feeding tube cap may split or fail to close properly. You should notify your physician if this develops.
❈ How is a PEG tube removed?
PEG tube removal should only be done by a trained healthcare provider. If the brand of tube has a soft internal mushroom bolster, it can be removed by pulling. This may cause some transient stinging and burning at the incision site. If it has a balloon internal bolster, the balloon is deflated and the tube is removed. There are also unique commercial PEG brands that require other methods of removal.
Endoscopic Retrograde Cholangiopancreatography, commonly known as ERCP, is a minimally invasive medical procedure used to diagnose and treat problems in the bile ducts, gallbladder, and pancreas. It combines endoscopy and fluoroscopy to visualize and access these structures.
During an ERCP procedure, a flexible, lighted tube called an endoscope is passed through the mouth and guided down the esophagus, stomach, and into the duodenum (the first part of the small intestine). Once the endoscope reaches the ampulla of Vater (the opening where the bile duct and pancreatic duct join the small intestine), a small catheter is inserted through the endoscope and into the ampulla.
Through the catheter, a contrast dye is injected into the bile and pancreatic ducts, which helps highlight these structures on X-ray images taken using fluoroscopy. This allows the physician to identify any blockages, narrowings, or abnormalities in the ducts.
ERCP is not only a diagnostic tool but also a therapeutic one. If any obstructions or stones are found in the bile ducts, the doctor can perform interventions during the same procedure. For instance, they can use specialized tools passed through the endoscope to remove gallstones, place stents to open blocked ducts, or perform other procedures to improve the flow of bile and pancreatic fluids.
ERCP is commonly used to investigate conditions such as jaundice, pancreatitis, and unexplained abdominal pain. It is considered a safe procedure; however, like any medical intervention, there are risks involved, such as pancreatitis, infection, or bleeding. Your healthcare provider will carefully assess the risks and benefits before recommending ERCP.
Overall, ERCP plays a crucial role in the diagnosis and management of various conditions affecting the bile and pancreatic ducts, providing a less invasive alternative to traditional surgery in many cases. It continues to be an essential tool in modern gastroenterology, enabling healthcare professionals to offer effective treatment to patients with complex biliary and pancreatic disorders.
